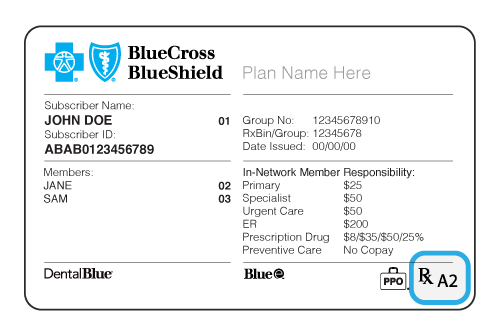
19101 Healthcare Management Services PO Box 3755. In WPA beginning on July 1 st 2019 all Highmark members in broad access products like PPO Blue and Blue Card will have full in-network access to all UPMC facilities and doctors.
Our vision is to ensure that all members of the community have access to affordable.
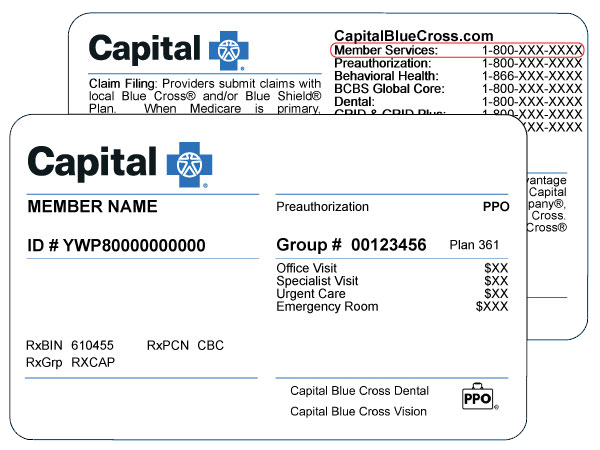
Blue shield managed care pa. If you have a grievance against your health plan you should first telephone your health plan at Los Angeles800 605-2556 TTY. An independent licensee of the Blue Cross and Blue Shield Association. Blue Shield of California Promise Health Plan complies with applicable state laws and federal civil rights laws and does not discriminate on the basis of race color national.
Pittsburgh PA 15230 Clinical Management Procedures In general when requesting coverage for a medication the following information in the bullet points below is required. This information applies to Medicaid members who have Blue Cross Community Health Plans BCCHP and Blue Cross Community MMAI Medicare-Medicaid PlanSM prescription drug benefits. Certified nurse midwives CNS.
17089-8125 Quality Care Admission Review PO Box 13499 1901 Market Street Philadelphia Pa. Box 3418 Scranto n PA 18505 ii Member Services. Highmarks mission is to be the leading health and wellness company in the communities we serve.
Blue Shield of California Promise Health Plan cumple con las leyes estatales y. Pennsylvania Blue Shield Customer Service Department PO Box 890052 Camp Hill Pa. The members primary care physician.
Each quarter BCBSTX holds a Community Advisory Committee CAC Meeting so that we can find out how we can serve you better. In WPA members in high performing or tiered products such as Community Blue Flex or Connect Blue are already in a high-quality lower cost plan. Blue Cross Blue Shield MT at 1-800-820-1674 or MUS EB at 1 -877-501-1722.
Blue Shield of California Promise Health Plan is a managed care organization wholly owned by Blue Shield of California offering Medi-Cal and Cal MediConnect Plans. Plus you get added benefits like routine dental vision and hearing care. To see examples of how this plan might cover costs for a sample medical situation see the next page.
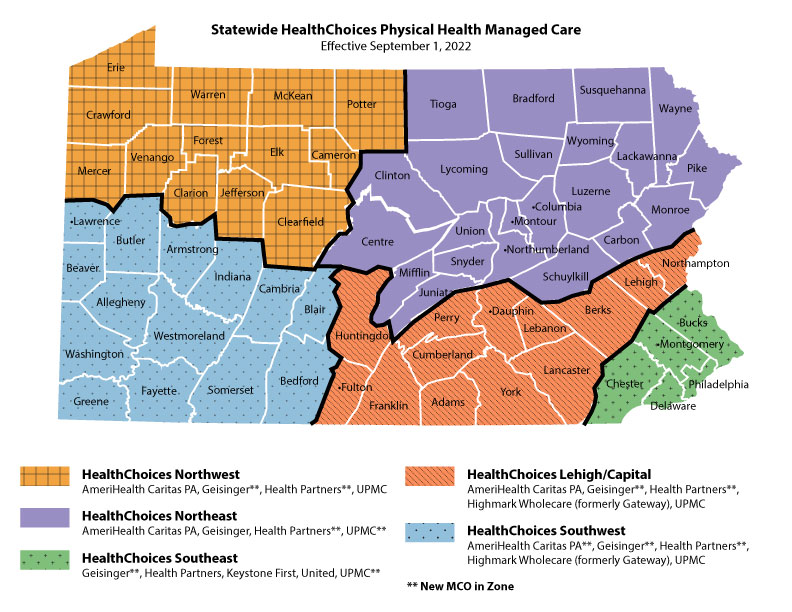
The Bureau of Managed Care also administers a consumer grievance program and ensures that each managed care plan has an approved process in place to handle member. Find authorization and referral forms. Section 10 Managed Care Referrals and Authorizations Central Region Products 102 Who can issue a referral The following parties can issue referrals.
Medicaid Managed Care Prior Authorization PA. If you would like to come and share your ideas with BCBSTX staff and community partners on what you like about your plan benefits or where we can do better please call the member advocate toll-free for details at 1-877-375-9097 TTY 711. For telephone PA requests or questions call 1-866-231-0847.
Highmark Blue Shield also provides services in conjunction with Blue Cross of Northeastern Pennsylvania in northeastern Pennsylvania and Independence Blue Cross in southeastern Pennsylvania. The Bureau of Managed Care identifies problems associated with cost quality and access within the managed care industry and initiates solutions with consumers and providers. 711 and use your health plans grievance process before contacting the department.
Blue Shield of California Promise Health Plan Medi-Cal and Cal MediConnect. A specialist authorized by Highmark Blue Shield to act as a members primary care physician. Non-Formulary Exception and Quantity Limit Exception PDF 129 KB Prior AuthorizationCoverage Determination Form PDF 136 KB Prior Authorization Generic Fax Form PDF 173 KB.
Non-Formulary Most products. Allow BlueCross BlueShield at least 24 hours to review this request. Blue Shield of California Promise Health Plan is a managed care organization wholly owned by Blue Shield of California offering Medi-Cal and Cal MediConnect Plans.
Questions about your rights this notice or assistance you can contact. Security Blue HMO-POS is a Mesidicare Advantage Health Maintenance Organization plan that covers all Medicare-covered benefits including preventive care doctor visits hospital stays and more. Blue Cross Community Managed Long Term Supports and Services MLTSS MLTSS refers to the delivery of long term supports and services through Managed Care Organizations.
It was designed to expand home and community based services provide better care. Documentation of a trial of at least two formulary products. Keystone First is Pennsylvanias largest Medical Assistance Medicaid managed care health plan serving more than 400000 Medical Assistance recipients in southeastern Pennsylvania including Bucks Chester Delaware Montgomery and Philadelphia counties.
The California Department of Managed Health Care is responsible for regulating health care service plans. Prime Therapeutics is the Pharmacy Benefit Manager PBM that provides drug benefits through Blue Cross and Blue Shield of Illinois BCBSIL. 17089-0035 For Blue Shield 65 Special inquiries.
Information on this website is issued by Highmark Blue Shield on behalf of these companies which serve the 21 counties of central Pennsylvania and the Lehigh Valley as full-service health plans.
 Prescription Drugs Drug Search Blue Cross Blue Shield Of North Carolina
Prescription Drugs Drug Search Blue Cross Blue Shield Of North Carolina
 Nys Medicaid Managed Care Pharmacy Benefit Information Center Faqs
Nys Medicaid Managed Care Pharmacy Benefit Information Center Faqs
Https Content Highmarkprc Com Files Educationmanuals Providermanual Hpm Chapter2 Unit6 Pdf
Https Www Highmarkblueshield Com Pdf File Pbs Prn Feb2002 Pdf
 Blue Cross Blue Shield Association Wikipedia
Blue Cross Blue Shield Association Wikipedia
 Nys Medicaid Managed Care Pharmacy Benefit Information Center Faqs
Nys Medicaid Managed Care Pharmacy Benefit Information Center Faqs
Blue Cross Blue Shield Of Texas 2021 Plan Guide Independent Health Agents
Https Digitalcommons Unf Edu Cgi Viewcontent Cgi Article 2705 Context Flablue Text
Http Www Bcbsnm Com Pdf Bma Prm Pdf




No comments:
Post a Comment
Note: Only a member of this blog may post a comment.