The prior authorization process is often complicated by a combination of factors including. CONTINUE SCROLLING OR CLICK HERE.
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
Lots of required steps each introducing the potential for delays and errors.
Prior authorization meaning. Prior authorization also known as precertification or prior approval is a process that many health insurance plans impose before they agree to pay for care. Medical Dictionary 2009 Farlex and Partners. Sometimes called prior authorization prior approval or precertification.
Enrich your vocabulary with the English Definition dictionary. Eligibility verification Prior Authorization Eligibility verification is important to ensure accurate and timely receipt of information regarding insurance coverage and determining the patients responsibility to pay for healthcare services. Prior Authorization means a decision by AvMed prior to the time a Health Care Service or other benefit is to be delivered that the Health Care Services are Medically Necessary.
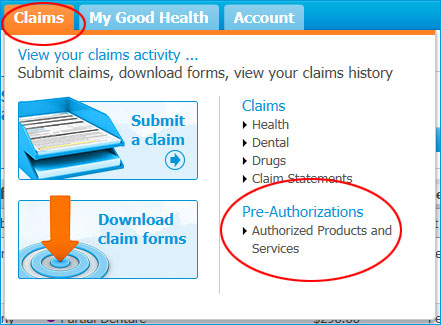
Prior Authorization is sometimes called pre-authorization prior approval or pre-certification. This approval is required in order for the insurer to pay the provider for the service. This allows insurers to.
Prior authorization is a health insurer or third partys approval for a health service or prescription before the patient receives it. Prior authorization is a requirement that your physician obtains approval from your healthcare provider before prescribing a specific medication for you or to performing a particular operation. A decision by your health insurer or plan that a health care service treatment plan prescription drug or durable medical equipment is medically necessary.
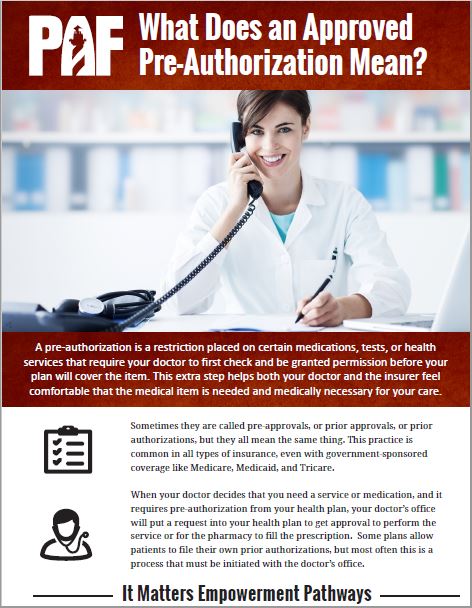
An authorization also known as a pre-approval or pre-certification is a formal request made to the insurance company before a procedure takes place. With prior authorization the physician or healthcare provider must get the insurance companys expressed approval for a particular drug or procedure or the insurer wont cover the cost. Official permission for something to happen or the act of giving someone official permission to.
Pre-authorization definition is - prior authorization. If youre facing a prior-authorization requirement also known as a pre-authorization requirement you must get your health plans permission before you receive the healthcare service or drug that requires it. In pharmacy a cost-containment procedure that requires a prescriber to obtain permission to prescibe a medication prior to prescribing it.
The approval by an insurer or other third-party payor of a health care service before the service is rendered. How to use pre-authorization in a sentence. Privacy Trust Info Prior authorization.
This approval is based on medical necessity medical appropriateness and benefit limits. If you dont get permission from your health plan your health insurance wont pay for the service. This request is made by the provider rendering the procedure.
Without this prior approval your health insurance provider may not pay for your medication or operation leaving you with the bill instead. Youll be stuck paying the bill yourself. Authorization as by an insurer that is required prior to performance of a health-care service such as a surgery or prescription of a drug.
Prior authorization is designed to help prevent you from being prescribed medications you may not need those that could interact dangerously with others you may be taking or those that are potentially addictive. Prior authorization definition in English dictionary prior authorization meaning synonyms see also priorPriorprior toprior probability. By Amanda DeMarzo December 15 2020 Prior authorization prior auth or PA is a management process used by insurance companies to determine if a prescribed product or service will be covered.
Prior authorization is a process required for the providers to determine coverage and obtain approval or authorization from an insurance carrier to pay for a proposed treatment or service. Its also a way for your health insurance company to manage costs for otherwise expensive medications. What is a Prior Authorization.
Also called prior approval. Participation by both payers and providers each of whom have different motivations workflows and infrastructure. This means if the product or service will be paid for in full or in part.
 Prior Authorization For High Cost Drugs
Prior Authorization For High Cost Drugs
 Importance Of Preauthorization In Revenue Cycle Management Rcm
Importance Of Preauthorization In Revenue Cycle Management Rcm
 Prior Authorizations And How To Get Your Medication Covered
Prior Authorizations And How To Get Your Medication Covered
 Definitions And Meanings Of Health Care And Health Insurance Terms
Definitions And Meanings Of Health Care And Health Insurance Terms
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
 Importance Of Preauthorization In Revenue Cycle Management Rcm
Importance Of Preauthorization In Revenue Cycle Management Rcm
 How To Obtain Prior Authorizations Jdrf
How To Obtain Prior Authorizations Jdrf
 Authorization Vs Pre Authorization What S The Difference
Authorization Vs Pre Authorization What S The Difference
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
 What Does An Approved Pre Authorization Mean Patient Advocate Foundation
What Does An Approved Pre Authorization Mean Patient Advocate Foundation
/prescription-56a68fa63df78cf7728eff7e.jpg)

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.